What are Streptococcal infections?
Image credit: NIH Image Gallery, Via Flickr
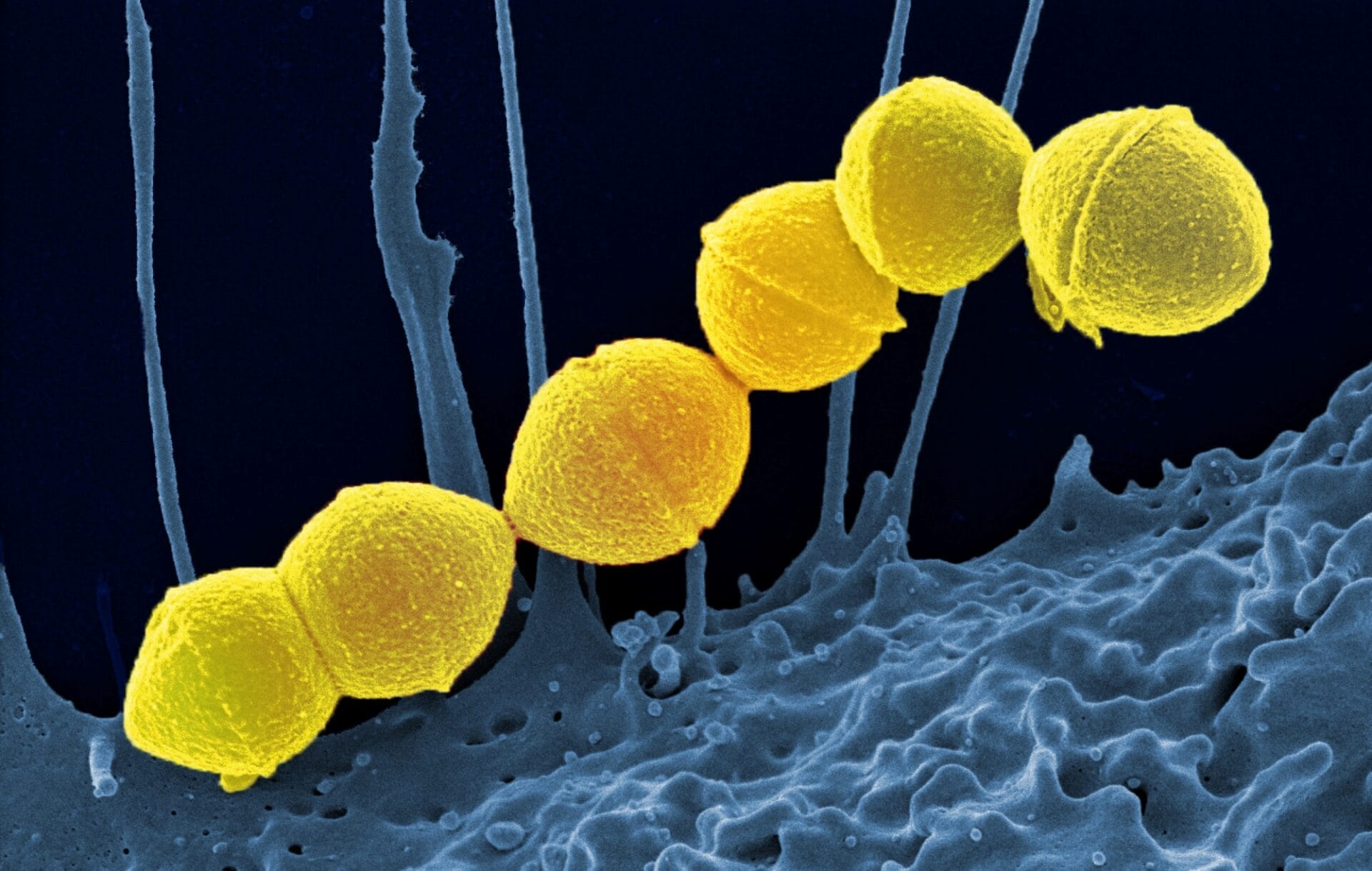
Streptococcal infections are any type of infection caused by the group of bacteria Streptococcus.
- Streptococcal infections are caused by the group of bacteria Streptococcus.
- There are many different types of streptococci and infections vary in severity from mild throat infections to pneumonia.
- The different types of Streptococcus bacteria also vary in where they live in the body and the way they are transmitted.
What are Streptococcal infections?
- Streptococcal infections are caused by the group of bacteria Streptococcus – a broad group that can cause many different infections, ranging in severity from mild illnesses to very serious, life-threatening infections like pneumonia.
- Streptococcal infections are primarily treated with antibiotics.
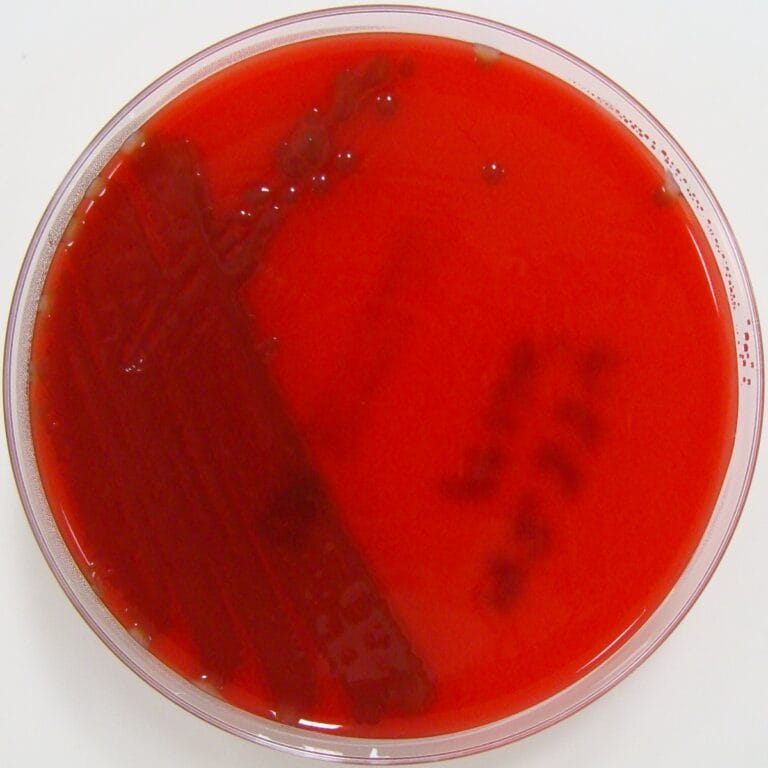
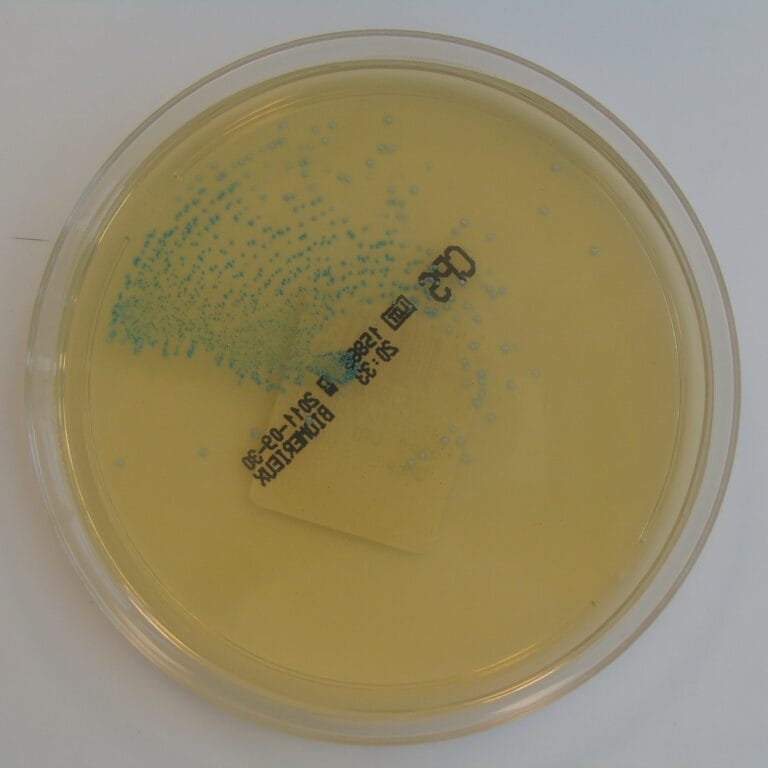
- Streptococci are divided into two key groups, based on how they look when grown on an agar plate:
- alpha (α)-haemolytic streptococci.
- beta (β)-haemolytic streptococci.
| A summary of Streptococcal bacteria described on this page | |
|---|---|
| Group | Subgroup |
| alpha (α)-haemolytic streptococci | Streptococcus pneumoniae - a single species with further subspecies |
| Viridans streptococci – a large group of different species of bacteria | |
| beta (β)-haemolytic streptococci | Group A streptococci (GAS) - typically species Streptococcus pyogenes |
| Group B streptococci (GBS) - typically species Streptococcus agalactiae | |
α-haemolytic Streptococci
- Many strains of α-haemolytic streptococci live naturally in humans causing no symptoms.
- α-haemolytic streptococci are split into two groups:
- Streptococcus pneumoniae – a single species of bacteria, which can be divided into subtypes.
- Viridans streptococci – a large group of different species of bacteria.
Streptococcus pneumoniae
- S. pneumoniae is usually found on the surface of the skin and inside the throat.
- It is transmitted through coughs and sneezes and causes infections in both adults and children.
- Minor infections can be treated relatively easily with antibiotics and include:
- sinusitis (inflammation of the sinuses).
- middle ear infections.
- More invasive infections pose a more serious threat to health and include:
- pneumonia (inflammation of the tissue in the lungs).
- meningitis (inflammation of the membranes covering the brain and spinal cord).
- bacteraemia (infection of the blood).
- People at the highest risk of invasive S pneumoniae infections are:
- babies under six months old.
- adults over 75 years old.
- adults with a weak immune system.
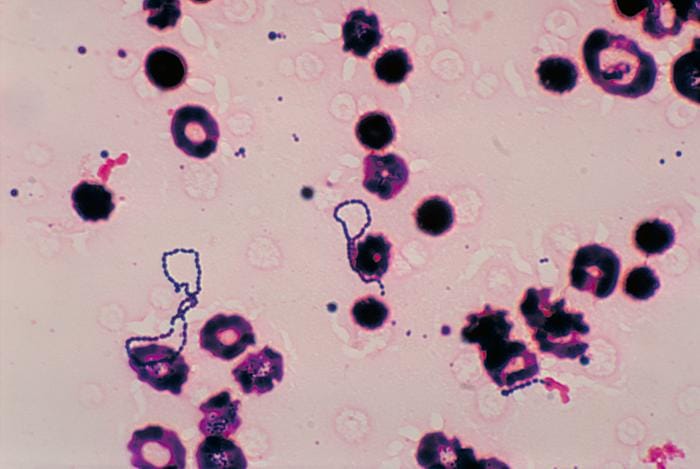
Viridans streptococci
- This group of α-haemolytic Streptococci are most often found in the mouth, gut and genital region.
- The most serious Viridans infections occur when the bacteria enter other regions of the body. For example, if Viridans get into the bloodstream it can cause endocarditis (infection of the inner lining of the heart).
- Individuals with damaged heart valves or cardiac abnormalities and compromised immune systems are at particular risk.
- Symptoms include, tiredness, weakness, fever, weight loss, respiratory problems and problems with heart function in cases where endocarditis occurs.
How are α-haemolytic streptococci infections diagnosed and treated?
- Minor infections can be diagnosed by taking a sample of saliva or a swab of the affected tissue and testing for the presence of streptococcal bacteria.
- Minor infections may not require treatment or may be treated with antibiotics.
- For invasive infections, additional tests may be required, such as a blood test for bacteraemia or cerebral spinal fluid test for meningitis.
- Invasive infections usually result in a hospital stay.
- Severe invasive infections may require intensive treatment with intravenous antibiotics for 7-10 days. In some cases, surgery may be required to remove or repair damaged tissue.
β-haemolytic Streptococci
- β-haemolytic Streptococci are further divided into two groups: Group A streptococci (GAS) and Group B streptococci (GBS).
- Group A are typically the species Streptococcus pyogenes. Group B are typically the species Streptococcus agalactiae.
Group A β-haemolytic streptococci (Streptococcus pyogenes)
- Streptococcus pyogenes is transmitted through coughs, sneezes or direct contact.
- Its infections can be either non-invasive or invasive (spread into the bloodstream and to other body sites).
- The most common of non-invasive infections include:
- strep throat: sore throat specifically caused by streptococcal infection.
- impetigo: contagious skin infection that causes sores and blisters.
- scarlet fever: infectious disease causing a sore throat and characteristic red rash.
- Invasive infections are much rarer and occur when the bacteria infect other areas of the body such as the blood and organs. This can result in:
- pneumonia: inflammation of the tissue in the lungs.
- bacteraemia: infection of the blood.
- necrotising fasciitis: flesh-eating disease.
- Left untreated, potential complications of Group A infection include rheumatic fever, a disease that affects the joints, kidneys and heart.

Group B β-haemolytic streptococci (Streptococcus agalactiae)
- Streptococcus agalactiae usually lives harmlessly inside the digestive system and genitals.
- It can be transmitted sexually or from mother to baby during birth.
- Group B β-haemolytic streptococci tend to only affect newborn babies as the bacteria can be passed onto the baby through the amniotic fluid (the protective fluid that surrounds the baby in the womb).
- Due to being continually exposed to it through our lifetimes, most people quickly develop a natural immunity to Group B β-haemolytic Streptococcus.
- Symptoms of group B β-haemolytic streptococcal infection in a newborn baby include:
- being floppy and unresponsive.
- poor feeding.
- unusually high or low body temperature.
- unusually fast or slow heart rate.
- If left untreated, group B β-haemolytic streptococcal infections can also lead to much more serious conditions such as meningitis and pneumonia. In severe cases, the infection can result in the baby being stillborn.
- Factors increasing risk of group B β-haemolytic streptococcal infection in new-born babies include:
- premature birth.
- being part of a multiple birth.
- having a mother with a history of group B streptococcal infection.
How are Group B β-haemolytic streptococci infections diagnosed and treated?
- These infections are diagnosed by a blood, urine or cerebral spinal fluid sample to identify the bacteria.
- A culture of fluid from the vagina or rectum can also determine if an individual is infected.
- The infection is treated with antibiotics, often directly into the bloodstream (intravenously).
- Treatment of these infections may require a hospital stay.
Preventing Group B Streptococcal infection in newborns
- Healthcare professionals take measures during labour and after birth to prevent newborns becoming infected with Streptococcus.
- If a baby is known to be at risk of Streptococcus infection, antibiotic injections are given to the mother during labour or to the baby shortly after birth.