What is colorectal cancer?
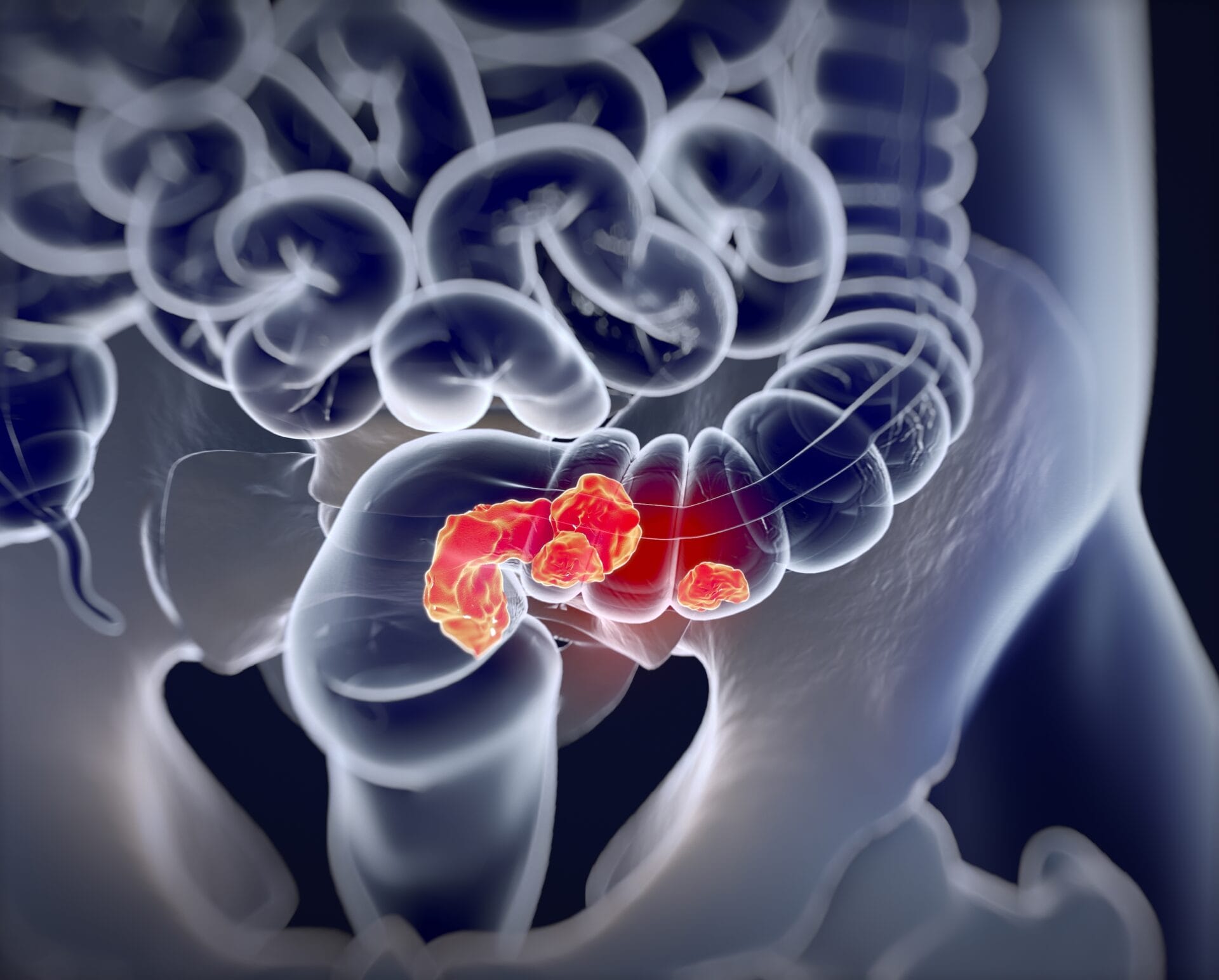
Colorectal cancer, also known as bowel cancer, is a complex condition that’s influenced by multiple genes and environmental factors.
- Colorectal cancer, or bowel cancer, is cancer that starts in either the large bowel (colon) or back passage (rectum).
- Each year in the UK, around 42,000 people are diagnosed with colorectal cancer. It’s the 4th most common cancer in the UK.
- Risk factors for colorectal cancer include age, family history, lifestyle factors and other medical conditions.
What is colorectal cancer?
- Colorectal cancer, or bowel cancer, is cancer that starts in the large bowel – which is made up of the colon and rectum.
- We don’t know what causes most colorectal cancers and most are sporadic. This means they are not linked to family history.
- In sporadic cancer, mutations are ‘acquired’ over time in cancer-causing genes, rather than inherited. For example, around 70-80% of people who develop colorectal cancer have a mutation in the APC gene. Around 15% of people have mutations in DNA repair genes.
- People may have mutations in more than one gene and research is still underway to find out more about the genetic causes of colorectal cancer.
- A strong family history of colorectal cancer can increase a person’s risk of the condition.
- Up to 30% of cases are linked to family history. This can be broken down into two groups:
- Hereditary colorectal cancer, where a known cancer-causing mutation has been passed between generations. The most common hereditary colorectal cancers are familial adenomatous polyposis and hereditary non-polyposis colorectal cancer.
- Familial colorectal cancer, when the condition clusters in the same biological family but doesn’t appear to be caused by a single gene. This is thought to be caused by multiple factors that cause changes to an individual’s DNA to increase their susceptibility to the disease.
What causes colorectal cancer?
- A person’s individual risk of colorectal cancer depends on their age, family history, lifestyle factors and other medical conditions. Having one or more risk factors doesn’t necessarily mean that a person will develop colorectal cancer.
- For example, people with a history of adenomatous polyps, inflammatory bowel syndrome or a previous colorectal cancer diagnosis might have an increased risk of developing the condition.
- Smoking tobacco has been shown to increase a person’s risk of developing colorectal cancer. It’s difficult to research the link between diet and cancer, but eating lots of red and processed meat can increase a person’s risk of colorectal cancer. Eating too little fibre can also increase a person’s risk.
- Being physically active and eating a balanced diet can help to reduce a person’s risk of colorectal cancer.
- Researchers are also learning about the role of the microbiome – the collection of bacteria, viruses and fungi everyone has living in and around their bodies. For example, some bacteria have been shown to cause the condition, while others have a preventative effect.
What are the symptoms of colorectal cancer?
- The symptoms of colorectal cancer vary with the location and size of the cancer. They are often a sign of another condition rather than cancer but it’s always important to check any new symptoms out with a doctor.
- Common colorectal cancer symptoms include:
- blood present in poo.
- a persistent change in bowel habits, including alternating between diarrhoea and constipation.
- the sensation of being unable to empty the bowels, despite going to the toilet.
- unexplained weight loss.
- tiredness, which can be caused by a reduction in red blood cells as a result of bleeding.
How is colorectal cancer diagnosed?
- Most people with symptoms of colorectal cancer start with a visit to the GP, who decides which tests need to be done, including sending different samples to be analysed and carrying out a physical examination.
- Colorectal cancer is usually confirmed with a colonoscopy, which enables the doctor to look at the whole colon and take small samples (biopsies) of any suspected tumours if necessary.
- The UK has screening programmes that look for early stage bowel cancers or abnormalities that could lead to cancer. This is an at-home test that looks for tiny traces of blood in a person’s poo.
- The age of eligibility for screening varies across the UK. Some people who are at higher risk of colorectal cancer might have screening at an earlier age.
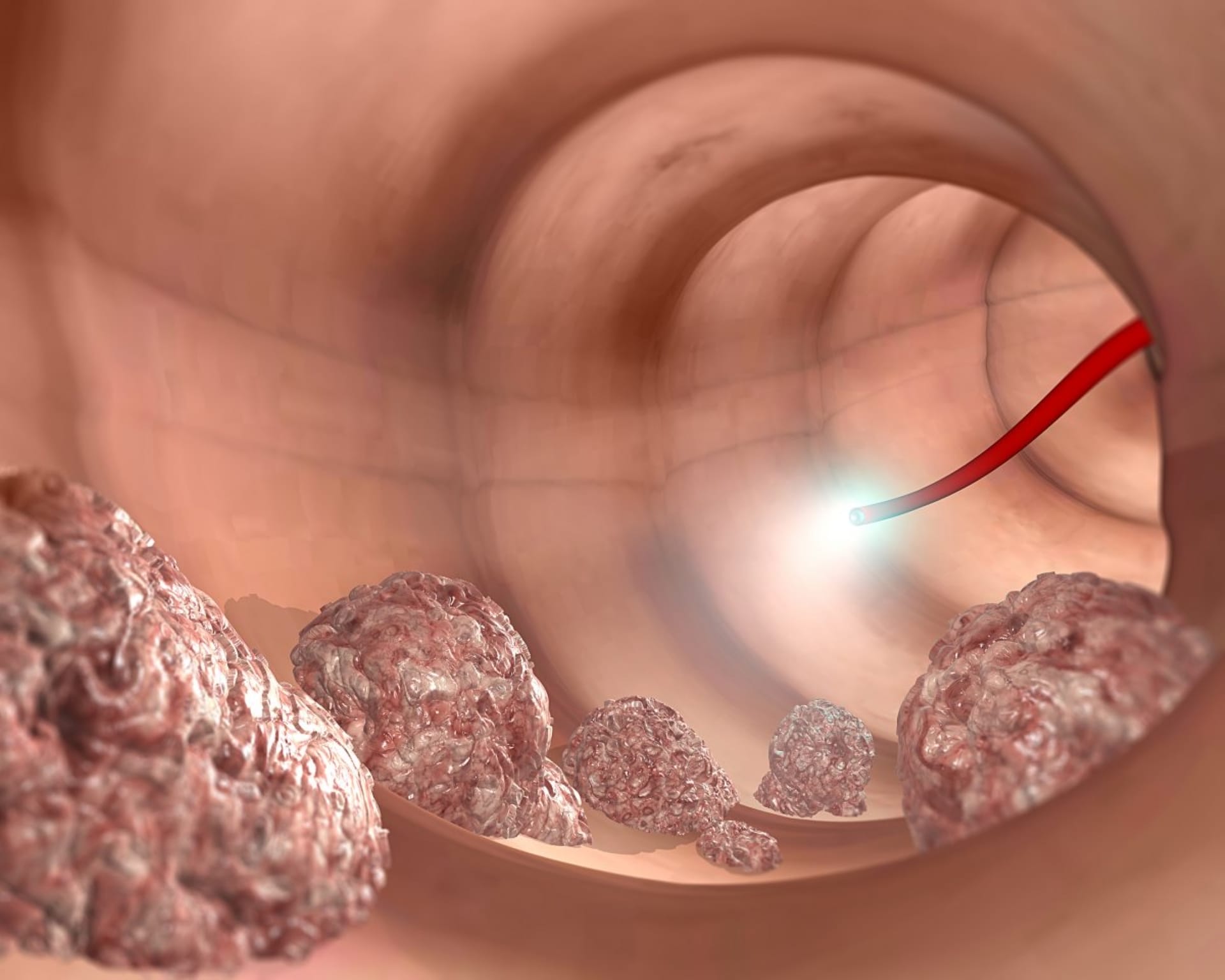
Representation of a colonoscopy examination to identify tumours. Image credit: Shutterstock.
How is colorectal cancer treated?
- Treatment for colorectal cancer is more likely to be successful if the condition has been diagnosed early, before it has had the chance to spread.
- Treatment depends on the location, size and spread of the cancer, as well as the patient’s health and personal choice.
- Early stage colorectal cancer can be treated effectively with a surgical procedure called local resection. This involves removing the cancer from the bowel lining as well as a border of healthy tissue from around the cancer. This is sometimes performed with a colonoscopy or by keyhole surgery.
- In more advanced cases, surgery may involve removal of a section of the colon containing the tumour. This procedure is called a colectomy.
- Combined chemotherapy and radiotherapy is sometimes used before surgery to shrink the tumour and make it easier to remove. Chemotherapy may also be used instead of or after surgery to kill any remaining cancer cells.
- Some people with advanced colorectal cancer are treated to relieve their symptoms.
- New therapies are currently being developed to help target the cancerous cells more specifically and better treat people with colorectal cancer. New treatments are always in clinical trials before being rolled out to all eligible patients.