What is hereditary haemochromatosis?
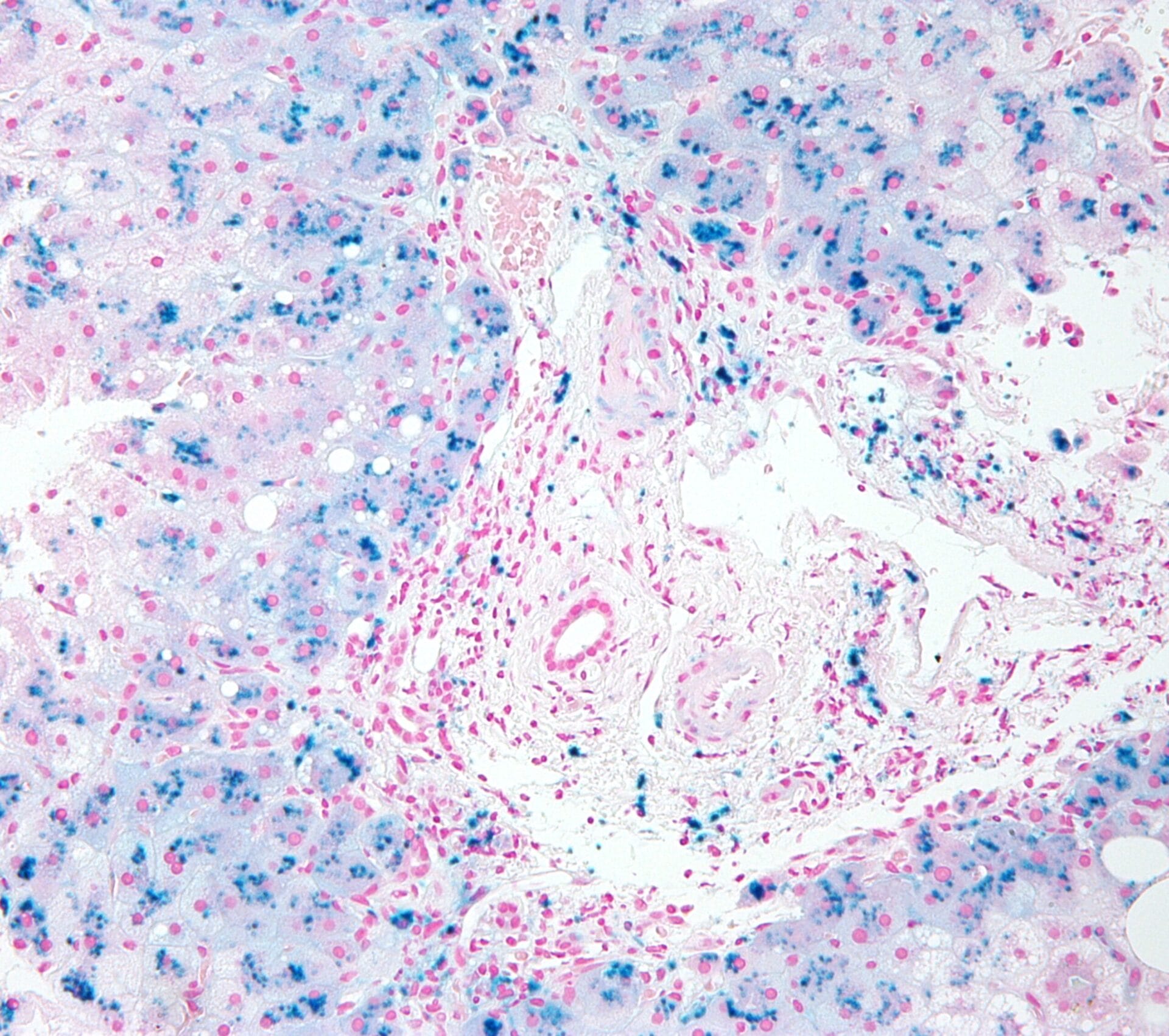
Image credit: Nephron / via Wikimedia Commons
Hereditary haemochromatosis is an inherited condition in which iron accumulates in the blood, often because too much iron is absorbed from food during digestion.
- Hereditary haemochromatosis is also known as iron overload disease.
- It is an inherited disorder in which iron accumulates in the blood, which can damage tissues and organs in the body.
- It is classified by type depending on the age of onset, whether the condition was inherited and the genetic cause.
What is hereditary haemochromatosis?
- Hereditary haemochromatosis is a single gene condition, classified by type depending on the age of onset, whether it was inherited or the genetic cause:
- Type 1 haemochromatosis, the most common type, is caused by mutations in the High Iron Fe (HFE) gene on chromosome 6. 93% of hereditary cases are caused by mutations in this gene.
- Type 2 haemochromatosis is caused by mutations in either the HFE2 or HAMP genes.
- Type 3 haemochromatosis is caused by mutations in the TFR2 gene.
- Type 4 haemochromatosis is caused by mutations in the SLC40A1 gene.
What is the biology of hereditary haemochromatosis?
- The HFE, HFE2, HAMP, SLC40A1 and TFR2 genes are all involved in regulating the absorption, transport and storage of iron in the body.
- For example, the HFE gene codes for a protein found in the membranes of the small intestine – the part of the gut where iron is absorbed from food.
- A mutation in any of these genes impairs the body’s ability to control iron absorption during digestion and manage the distribution of iron to parts of the body where it is needed.
- The result is that excessive amounts of iron are absorbed from the food and deposited in various organs, such as the liver, heart and pancreas.
- Since humans cannot increase the removal of iron from the body, excess iron can overload tissues and organs, leading to damage, and more serious conditions like liver cancer.
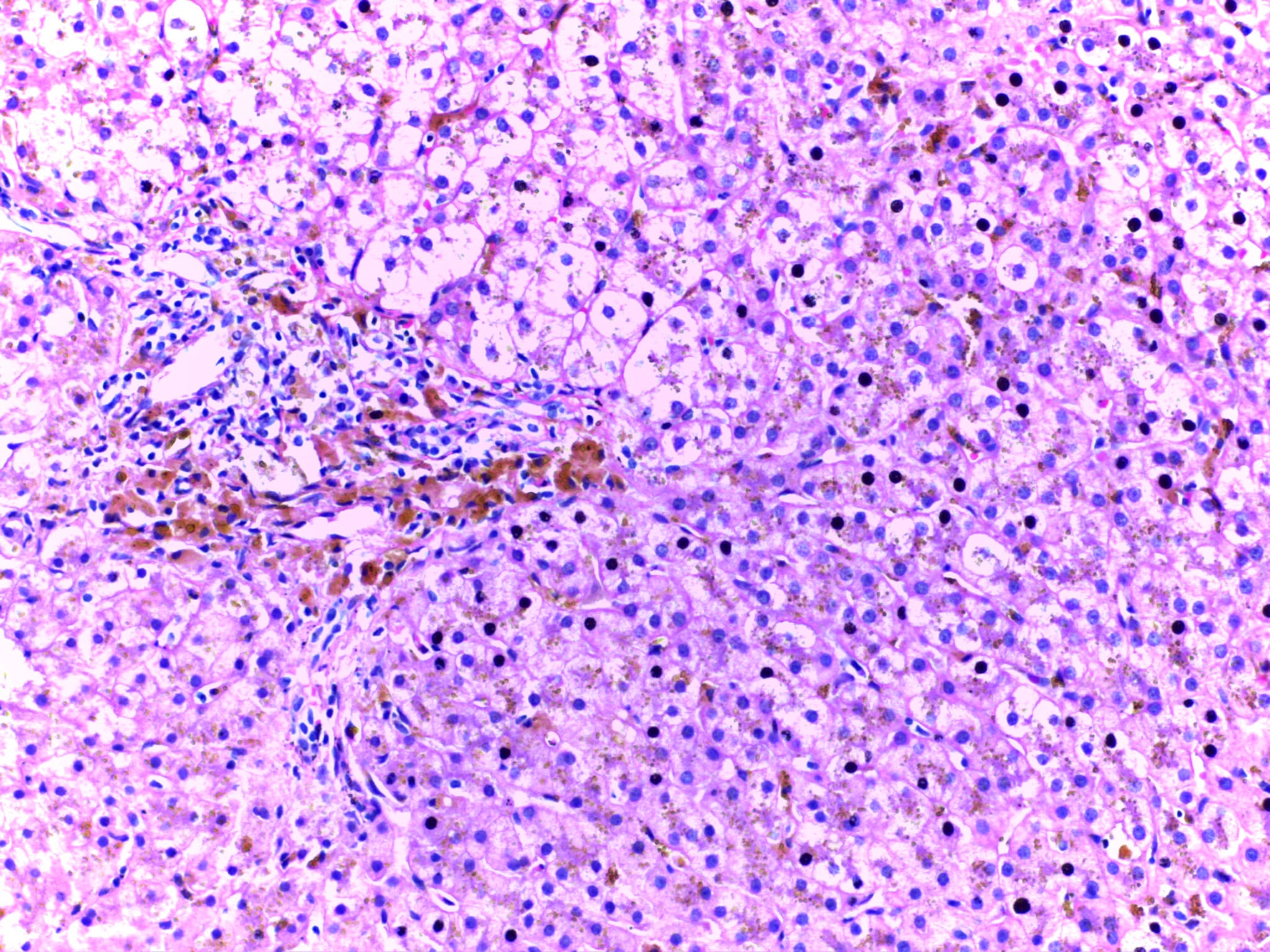
Microscope image of a haemochromatosis liver, showing stored iron deposits in yellow/gold. Image credit: Calicut Medical College / via WikiMedia Commons
What are the symptoms of hereditary haemochromatosis?
- The onset of symptoms depends on the type of haemochromatosis:
- Type 1 and 4 are adult onset.
- Type 2 is juvenile onset (meaning it develops in childhood).
- Type 3 usually presents before the patient is 30 years old.
- Early symptoms of hereditary haemochromatosis include fatigue, weakness, impotence and pain in the abdomen and joints.
- Later symptoms of the disease can include liver damage or liver cancer, diabetes, heart disease and arthritis. Many people with haemochromatosis are unaware they have the disease until it has reached these more dangerous, advanced stages.
- Some people also experience shrinking of the testes or ovaries and pituitary gland, which are responsible for making different hormones.
- People who menstruate are less likely to develop severe symptoms, because they generally lose more iron from the body. The same is true during pregnancy and lactation.
How is hereditary haemochromatosis diagnosed?
- A person’s DNA can be tested for mutations in the HFE gene.
- Hereditary haemochromatosis can be detected before the onset of symptoms by looking at the levels of iron in the blood.
- For example, the transferrin saturation test measures the total level of iron in the blood, compared to the body’s capacity to store the iron. A serum ferritin test may also be carried out, to measure the levels of ferritin – a protein which stores iron in the blood. High serum ferritin can indicate a person has high levels of iron in the blood.
How is hereditary haemochromatosis treated?
- Red blood cells are full of the protein haemoglobin, which contains iron. Removing up to a pint of blood at regular (usually weekly) intervals can reduce the number of red blood cells and stimulate the body to produce more.
- This draws on the body’s iron reserves to make more haemoglobin within the cells, reducing the amount of iron in the blood.