Pharmacogenomics and cancer

Pharmacogenomics is a form of personalised medicine, where the dose and type of drug given to a person is decided based on their genetic makeup.
Key terms
Pharmacogenomics
An area of genomics that studies how individuals react to drug treatments - a form of personalised medicine.
Gene
A section of DNA within a genome that carries a specific set of information - often the information needed to make a protein.
DNA
(deoxyribonucleic acid) A molecule that carries the genetic information necessary to build and maintain an organism.
- Cancer is a genetic disease where mutations in DNA cause cells to grow and divide out of control, forming tumours.
- Using pharmacogenomics, drugs can be targeted to specific genetic mutations within cancer cells.
- Here, we look at how doctors are using pharmacogenomics to match people with cancer to the best treatment for them.
Herceptin and breast cancer
Herceptin® (also known as trastuzumab) is a drug used in the treatment of breast cancer.
Research has shown us that there are at least 10 different types of breast cancer. Each of these are caused by different genetics and biology, and so respond differently to treatments.
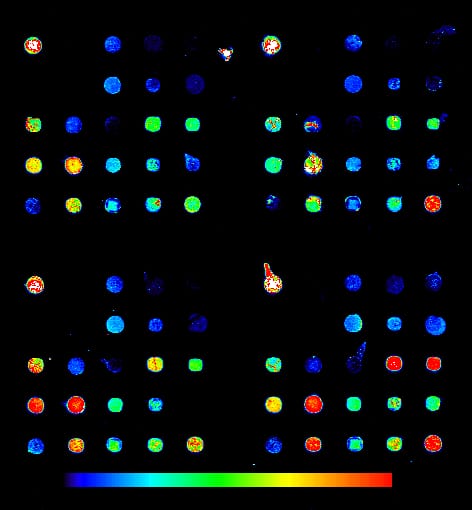
For example, around 1 in 5 breast cancers have high levels of HER2 on the surface of their cells. Herceptin is a drug that targets the HER2 protein and can be a highly effective treatment for people with this type of breast cancer. It is very unlikely to work in people without lots of HER2 on their cancer cells.
Having high levels of HER2 is called being ‘HER2-positive’. A genetic test can help determine if a patient’s cancer is HER2-positive and whether Herceptin is a suitable treatment for their cancer.
Glivec and leukaemia
Glivec® (also known as imatinib) is a targeted treatment for chronic myelogenous leukaemia (CML).
Chronic myelogenous leukaemia (CML) is a type of leukaemia blood cancer. It’s often caused by a mutation that causes a transfer of the ABL gene on chromosome 9 onto chromosome 22. This is called the ‘Philadelphia chromosome’ and results in the ABL and BCR genes joining together on chromosome 22 to make a fusion gene, called BCR-ABL.
Typically, the ABL gene codes for an enzyme called a tyrosine kinase, which helps cells to send signals to each other and control growth and division. The BCR-ABL fusion gene also codes for a similar enzyme – but the signals are not regulated in any way.
This can cause white blood cells to divide quickly and continuously, leading to massive numbers of cells being produced. This is a characteristic of chronic myeloid leukaemia and leads to symptoms such as fatigue, appetite loss and fever.
The drug Glivec®, or imatinib, is a tyrosine kinase inhibitor. It can recognise and target this specific BCR-ABL fusion protein, so can be used to block cancer cell growth in people with CML who have the Philadelphia chromosome.
Rituximab and lymphoma
Rituximab (also known as Mabthera) is a type of targeted treatment for people with certain types of lymphoma or leukaemia.
Rituximab is a type of treatment called an ‘immunotherapy’, which helps the immune system track down and attack cancer cells.
Lymphoma and leukaemia blood cancer cells are often very good at hiding from the immune system. However, some types of these cancers have high levels of a molecule called CD20 on their surfaces.
Rituximab works by attaching itself to every CD20 protein that it can find, acting like a flag for the immune system. The cells of the immune system are then able to pick out the marked cancer cells and destroy them.
The future of cancer therapy
A hallmark of cancer cells is that they divide rapidly. Many current chemotherapy drugs target dividing rapidly cells whether they are cancer cells or not. This is why some chemotherapy drugs cause hair loss as they kill the cells of the hair follicles that normally divide a lot. Similarly, gut cells divide rapidly, so chemotherapy can cause sickness.
A benefit of targeted therapies for cancer is that they can be designed to target only characteristics that are specific to cancer. This will hopefully lead to more effective treatments with far fewer side effects.