What is malaria?

A global public health challenge, malaria is one of the most common infectious diseases in the world.
- Malaria is a life-threatening disease caused by the Plasmodium parasite, which is transmitted through the bite of infected mosquitoes.
- It’s predominantly found in the tropical and subtropical areas of Africa, South America and Asia.
- If not detected and treated promptly, malaria can be fatal. However, with the right treatment, started early enough, it can be cured.
- In 2021 and 2023, two vaccines were approved to help prevent malaria in high risk areas.
What is malaria?
- Malaria is a life-threatening disease caused by a microscopic, single-celled parasite, called Plasmodium.
- The parasite is transmitted through the bite of infected female Anopheles mosquitoes.
- Malaria can be fatal if it’s not detected and treated promptly. However, with the right treatment taken as early as possible, it can be cured.
- Malaria is predominantly found in the tropical and subtropical areas of Africa, South America and Asia.
- There are six different species of malaria parasite that cause malaria in humans: Plasmodium falciparum, Plasmodium vivax, Plasmodium ovale curtisi, Plasmodium ovale wallikeri, Plasmodium malariae and the very rare Plasmodium knowlesi.
- Plasmodium falciparum is one of the most common and causes the most serious, life-threatening infections in humans.
- There are more than 100 kinds of Plasmodium that can infect many animal species such as reptiles, birds and mammals.
How many people are affected by malaria?
- In 2021, it was estimated that there were 247 million cases of malaria around the world, and 619,000 deaths.
- Around 95% of deaths are in children under the age of five living in Sub-Saharan Africa.
- Between 2000 and 2015, the mortality rate for people with malaria dropped by 47%.
- These mortality rates increased slightly during the Covid-19 pandemic, in part due to the increased challenges faced by healthcare providers.
- Malaria is most severe in villages that are surrounded by forests, where rainfall patterns and humidity levels suit the mosquito. Transmission occurs mostly during the rainy season, but rates of transmission can vary from one year to the next.
- Malaria was endemic in the UK until the 19th century but was eradicated and is no longer spread in the UK.
Image credit: World Health Organization (via World Bank) – processed by Our World in Data.
How is malaria transmitted?
- Malaria is generally transmitted via the bite of the female Anopheles mosquito. There are about 20 different Anopheles species that are responsible for the spread of malaria between humans.
- If a mosquito bites a person already infected with the malaria parasite, it can suck up the parasite in the blood and transmit the parasite to the next person bitten.
- Malaria is generally not spread directly from person to person – although in some rare cases, it has been spread through blood transfusions and the sharing of needles.

The life cycle of the malaria parasite, Plasmodium
- The malaria life cycle starts when a mosquito carrying the malaria parasite bites a human, injecting the parasite in its saliva into the human bloodstream.
- At this point, the parasite is in its sporozoite form. Once injected into the bloodstream, the parasite heads for the liver and – usually within 30 minutes – invades the liver cells.
- Within the liver cells, the parasite transitions into a new form – called a merozoite – and multiplies thousands of times. Some species live dormant here for months or years, but most are in the liver for 10 days.
- Eventually, the parasite bursts out of the liver and invades the red blood cells in the bloodstream, multiplying further.
- After around 48 hours, the cells are so full of parasites that they burst – releasing the parasite into the bloodstream to infect more cells.
- Over 10 days, the parasite develops into the immature sexual form, called a gametocyte, and is ready to move into the next stage of its life cycle in the mosquito. This is the form that the mosquito takes up when it bites an infected human.
- Once inside the mosquito gut, the parasite matures into a gamete.
- Gametes fuse together during sexual reproduction, resulting in offspring that burrows through the mosquito’s stomach wall. On the other side of the stomach wall, the offspring forms an oocyst – within which thousands of new sporozoites form.
- The new sporozoites are released from the burst oocyte after about 5 to 7 days. These then migrate up to the mosquito’s salivary gland, ready to be injected into the next individual it bites.
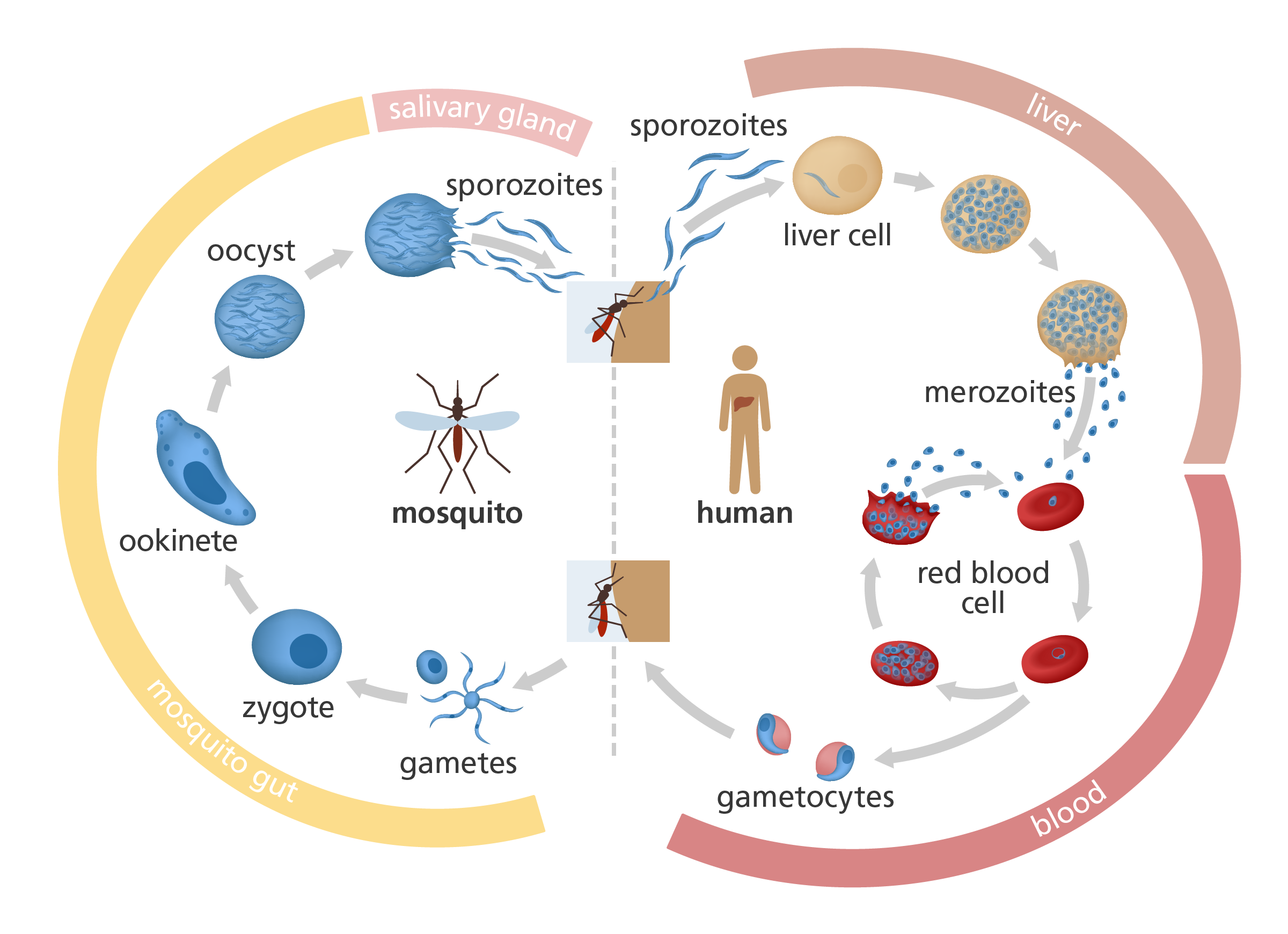
An illustration to show the life cycle of the malaria parasite. Image credit: Laura Olivares Boldú / Wellcome Connecting Science
What are the symptoms of malaria?
- Malaria symptoms usually appear after seven to 18 days – the time it takes for the parasite to infect and burst the red blood cells.
- Symptoms are flu-like, including fever, sweating, shivering, aching, nausea and headache.
- New red blood cells are infected and burst every 48 – 72 hours, resulting in another wave of symptoms that last six to 10 hours.
- Some species of parasite – such as Plasmodium vivax and Plasmodium ovale – can lie dormant in the liver and take up to a year for symptoms to develop.
- Destruction of the red blood cells can also lead to anaemia.
Complications associated with malaria
- The type and severity of symptoms depends on which type of malaria parasite someone is infected with. All cases of Plasmodium falciparum malaria are potentially severe and life threatening.
- In severe Plasmodium falciparum infections, parasite-filled red blood cells can block circulation to major organs. This can result in serious complications such as:
- cerebral malaria: the brain swells, potentially causing seizures, coma, permanent brain damage or death.
- liver failure and jaundice: the liver is prevented from performing its normal functions leading to a build-up of toxins in the body. These toxins tend to cause the skin and whites of the eyes to go a yellow colour.
- pulmonary oedema: a build-up of fluid in the lungs causes breathlessness and can potentially stop the lungs from functioning – resulting in high levels of carbon dioxide and low levels of oxygen in the blood.
- kidney failure: caused by a build-up of waste products in the body, leading to weakness and shortness of breath.
- acidosis: the blood becomes dangerously acidic due to the release of toxic compounds from bursting red blood cells.
- tropical splenomegaly: the spleen swells and becomes overwhelmed by clearing infected red blood cells from the blood. Eventually the spleen can become blocked and stop functioning, leaving a person vulnerable to other infections.
- A major reason for complications is because of missed or delayed diagnosis. Early diagnosis and prompt treatment can often help avoid complications like these.
How is malaria diagnosed?
- Often, if a child living in a country with a high prevalence of malaria develops a high fever, they will be taken to hospital on the assumption that they have malaria.
- The most accurate way to diagnose malaria is by taking a drop of blood, smearing it on a slide and then examining it under a microscope to look for malaria parasites inside the red blood cells.
- This relies on the availability of a clinic with a microscope, electricity and a trained technician to look at the slides – things which are not always readily available in many countries with high levels of malaria.
- Rapid diagnostic tests involve dipping a test stick into a drop of blood to test for the presence of the parasite. If the parasite is present in the blood, sample bands appear on the test stick – a bit like a pregnancy test or a Covid-19 test.
- Some rapid diagnostic tests are able to identify which species of Plasmodium is present. These are convenient as they eliminate the need for high-tech equipment and a result can be generated within 15 minutes.

A blood sample being dropped into a rapid diagnostic test for malaria. Image credit: USAID