How is malaria treated and prevented?

Malaria is a disease that is preventable and treatable when tackled early.
Before reading this page, you might want to read our introduction to malaria, here.
- If malaria is diagnosed and treated quickly, most people will recover fully.
- A major challenge in the treatment of malaria is that some species of malaria parasite are becoming resistant to treatment.
- Malaria prevention has significantly improved in recent decades and, in 2021 and 2023, two new preventative vaccines were approved for use in high-risk regions.
How is malaria treated?
- Most people fully recover from malaria, provided it has been diagnosed and treated quickly.
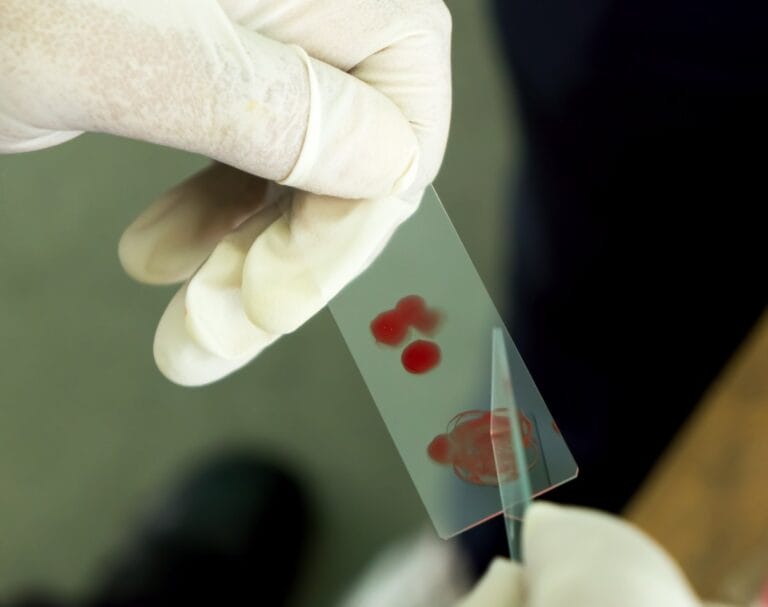
- Treatment usually takes the forms of ‘antimalarial’ drugs, which kill Plasmodium – the group of parasite species that can cause malaria. The exact treatment depends on the severity of the disease, the species that caused it and where in the world the infection was acquired.
- A major challenge is that around the world, the parasite that causes malaria – different species of Plasmodium – is becoming resistant to these treatments.
- Because of this, drugs are often used in combination with each other. For example, primaquine targets the liver phase of the parasite’s life cycle, while chloroquine targets the blood stages of the life cycle.
- A combination of drugs called ‘artemisinin-based combination therapy’ (ACT) is currently the main treatment for people with Plasmodium falciparum malaria – the most severe type of malaria. The fast-acting artemisinin first reduces the number of parasites, before the second partner drug eliminates any that are left.
- This is important to ensure the parasite is fully removed from the body, including any dormant parasites lying in the liver.
- You can read more about drug resistance in malaria here.
Some people develop partial natural immunity to the malaria parasite.
- Partial immunity can be developed over years of exposure to the disease. Although it never develops into full immunity it can reduce the severity of disease and risk of death from malaria.
- Most deaths caused by malaria occur in young children under five years. This is often because their bodies have not had a chance to develop any immunity to the parasite.
How can malaria be prevented?
Malaria is a disease that can be prevented. There are various strategies in place to help people avoid infection with the Plasmodium parasite.
Vaccines
- It took decades of research – but in 2019, the first vaccine against the malaria-causing Plasmodium falciparum parasite was approved.
- This was tested in pilot studies in 2019 and approved for wide-spread use in 2021 in high-risk areas of Africa, where levels of this parasite species are very high.
- The vaccine works by preventing the malaria parasite from entering the liver where it can mature and multiply to cause disease symptoms.
- In the years since, the vaccine has slowly been rolled out across high-risk areas, helping to reduce the numbers of children dying from severe malaria. A second vaccine was approved in 2023.
- The vaccine is not considered a ‘magic bullet’ against malaria but is an important building block towards the development of future malaria vaccines.
- You can read more about the long journey to a malaria vaccine here.
Vector control
- Anopheles mosquitoes are ‘vectors’ for malaria – meaning they transmit the disease between humans and other animal hosts.
- Vector control refers to methods that limit or eradicate malaria-carrying mosquitos. These strategies helped to reduce deaths from malaria by 47% between 2000 and 2015.
Vector control strategies include:
- Indoor residual spraying: spraying insecticide (a substance that kills insects), once or twice a year, on all indoor surfaces where mosquitoes are likely to rest. This has been found to reduce the survival of mosquitoes that enter the home.

Carrying out indoor residual spraying in Ghana. Image credit: Navrongo Health Research Centre, Ghana; Will Hamilton - Long-lasting insecticidal nets: mosquito nets that are also sprayed with an insecticide. They provide a physical and chemical barrier at night when the mosquito is most likely to bite and are very effective when used by entire communities.

A mosquito net hung over a bed to help protect against mosquito bites during the night. Image credit: Shutterstock - Larvicide: treating mosquito breeding sites with substances that kill the larval stages of the insect. It’s effective – but only in areas where mosquito breeding sites are fixed in one place and easy to find.
Preventative drugs
- Antimalarial drugs can also be used to prevent malaria and can reduce the risk of developing the condition by up to 90%.
- This is known as chemoprophylaxis, killing the blood stage of the malaria parasite and preventing the symptoms of the disease.
- The drugs used to prevent malaria will depend on the region and the most common parasite species. For example, chloroquine isn’t used to prevent P falciparum in Africa or Asia, because the parasite is resistant to chloroquine here.
- Preventative antimalarial drugs aren’t routinely given to everyone in high-risk regions, partly because it would risk causing further drug resistance.
- However, pregnant people living in moderate-to-high risk areas are given antimalarial drugs at regular intervals during their pregnancy, because malaria infections can be very dangerous for both the mother and the baby.
- During the seasons when malaria transmission is high, infants are usually given a monthly course of antimalarials alongside their routine medical care.
- It’s also recommended that people travelling to high-risk areas take antimalarial drugs, starting the course before entering the region to allow the medicine to increase to effective levels, and continuing after returning home to cover the incubation period.

Major challenges in malaria control
Drug resistance
- Drug resistance is a major challenge when treating malaria. It has led to several antimalarials no longer being used – in specific regions or around the world – because they are no longer effective.
- If a parasite becomes resistant to an antimalarial drug, it might take longer for a person’s symptoms to be relieved, or the drug might be completely ineffective at eliminating the parasite from the body.
- Drug resistance is further complicated by a process called cross-resistance. This is when resistance to one drug enables the parasite to be resistant to another drug that works by a similar mechanism.
- As outlined above, artemisinin combination treatments (ACTs) have been integral to the recent successes in global malaria control. But some parasites, including Plasmodium falciparum, are becoming resistant to artemisinin or this combination of treatments.
- Scientists are using genomics techniques to tackle drug resistance in these parasites which will hopefully prevent the spread of resistance. You can read more about this here.
- This includes the Malaria Cell Atlas. Developed by scientists at the Wellcome Sanger Institute, this is a comprehensive database of the genes of each of the Plasmodium species which can be used by scientists around the world to better understand how we can target the parasite.
Insecticide resistance
- Just as the parasite can become resistant to antimalarial drugs, the mosquitoes that carry the parasite can become resistant to the chemicals that are designed to kill them.
- Insecticide use is an important component of vector control – so resistance to insecticide is a real challenge in controlling malaria.
- Resistance develops when a mutation occurs in a mosquito’s DNA that makes it better at surviving contact with the insecticide.
- When the mosquito breeds, it passes the mutation onto its offspring, producing more mosquitoes that can survive the insecticide.
- The World Health Organization closely monitors insecticide resistance to help make decisions about how to manage the problem. For example, rotating different insecticides frequently can help to avoid mosquitoes becoming resistant to specific chemicals.
- Scientists are also using genomics to identify which genes are involved in insecticide resistance, which may lead to new ways to overcome it.


